Is it true that ancient physicians tasted human urine to determine if a patient had diabetes? Why did diabetics feel better in a besieged fortress? And how did dogs help create artificial insulin?
What is this disease?
Diabetes is a general term for diseases characterized by excessive urination. It comes from the Greek verb δῐᾰβαίνω — to flow, to pass through. The word δῐᾰβήτης is translated as “compass, carpenter’s rule, siphon.” It was probably the latter meaning that influenced the emergence of the medical term, since urine was excreted from the body too quickly.
There are two types of diabetes — diabetes mellitus and diabetes insipidus, as well as subtypes of diabetes such as renal glycosuria or gestational diabetes. They are all related in one way or another to the body’s ability to regulate blood glucose levels.
Between 1980 and 2014, the number of people with diabetes increased from 108 million to 422 million, while mortality increased by 3%. The prevalence of diabetes is increasing faster in low- and middle-income countries than in high-income countries.
There are two main mechanisms by which diabetes occurs: when the pancreas does not produce enough insulin (type 1), or when the body cannot effectively use the insulin that is produced (type 2).
The causes of type 1 diabetes are unknown. Doctors believe that type 1 diabetes is the body’s aggressive response to the insulin-producing cells in the pancreas, which prevents the hormone from entering the bloodstream. In type 2 diabetes, the body's cells lose their sensitivity to insulin, so they do not accept the glucose the insulin carries, and it remains in the blood in excessive amounts — or, for some reason, insulin no longer effectively regulates glucose production by the liver, causing blood sugar levels to rise. Factors that contribute to the development of type 2 diabetes include obesity, physical inactivity, and genetics.
It took a long time to understand the mechanics of glucose action on the human body. Today, there are still gaps in our understanding, but a colossal step forward has been made over the last few decades.
How has diabetes been explained in the past?
The concept of diabetes was introduced by the ancient Greek physician Aretaeus of Cappadocia (30–90 AD). He described a disease whose symptoms included excessive thirst, frequent urination, and weight loss:
“The course is the common one, namely, the kidneys and the bladder; for the patients never stop making water, but the flow is incessant, as if from the opening of aqueducts… The nature of the disease, then, is chronic, and it takes a long period to form; but the patient is short-lived, if the constitution of the disease be completely established; for the melting is rapid, the death speedy. Moreover, life is disgusting and painful; thirst, unquenchable; excessive drinking, which, however, is disproportionate to the large quantity of urine, for more urine is passed; and one cannot stop them either from drinking or making water. Or if for a time they abstain from drinking, their mouth becomes parched and their body dry; the viscera seems as if scorched up; they are affected with nausea, restlessness, and a burning thirst; and at no distant term they expire.”
Galen tried to explain as simply as possible why this happens. He noted that diabetes was associated with kidney weakness and called it "diarrhea of the urine" (diarrhea urinosa). This term became established in Byzantine sources that followed the ancient tradition.
In Indian medicine, diabetes was also closely associated with polyuria. In the 6th and 5th centuries BC, two famous Indian physicians, Sushruta and Charaka, described several diseases with a common pathology, including “sweet urine,” i.e., urine having a characteristic sweet taste. Patients also suffered from extreme thirst and bad breath.
In Chinese medicine, diabetes was called xiaoke, which can be translated as “thirsty piss.” Diabetes occurs due to a deficiency of Yin energy in the kidneys and lungs and "internal heat that consumes fluids, causing exhaustion and thirst.”
A new interpretation was proposed by Paracelsus (1493–1541). He experimented with patients' urine by evaporating it to leave a white residue. He believed that this residue was salt. It was this residue that he believed caused thirst and frequent urination.
In 1670, the Oxford scientist Thomas Willis was the first in European medicine to notice that some patients suffering from polyuria had a sweet taste to their urine, while others did not. The way he found it was quite prosaic: flies flew to some jars of urine, while others left them uninterested. It would be almost a hundred years later, in 1776, that Matthew Dobson would prove the presence of sugar in both urine and blood. What remained to be understood was what affected blood sugar levels.
Diabetes treatment
At various times, it was suggested that diabetes be treated with herbs, bloodletting, or opium. Diet was mandatory. The idea was to restore the nutrients lost through polyuria, so patients did not eat less, but the opposite. It is not difficult to guess that this resulted in even greater mortality.
In China, acupuncture has been suggested to treat diabetes. For example, if you have excessive thirst, it is better to use ginseng root, and in case of weakness and excessive urination, you should use a mixture consisting of sticky rehmannia (Rehmannia glutinosa), dogwood berries (Cornus sp.), water plantain (Alisma sp.), yam tubers (Dioscorea sp.), chasteberry (Vitex sp.), tree peony (Paeonia suffruticosa), poria fungus (Wolfiporia extensa), Chinese aconite (Aconitum carmichaelii), and wuhang (Cinnamomum aromaticum).
Avicenna (Ibn Sina, the famous 11th century Persian physician and philosopher) described diabetes in detail in The Canon of Medicine. To the usual features of the disease, such as increased appetite and excessive urination, Avicenna added sexual impotence. He suggested treating diabetes with lupine, fenugreek, and turmeric. It is noteworthy that the first work devoted exclusively to diabetes appeared in the Islamic East. It was written in the early 13th century in the Ayyubid state by ʿAbd al-Laṭīf al-Baghdādī. The treatise consisted of excerpts from the works of ancient and Syrian physicians with al-Baghdadi’s own comments.

Schelte a Bolswert. Healing of Innocent of Carthage by St. Augustine. 1586-1659. The patient was suffering from gangrene. / Wellcome Collection
A scientific breakthrough
In 1794, the German physician Johann Peter Frank officially distinguished between diabetes mellitus (i.e., honey diabetes) and diabetes insipidus. He cited a change in the blood as the main cause of the disease.
In fact, a few years earlier (1788), Thomas Cowley noticed interesting correlations with the shape of the pancreas in diabetics during a series of autopsies. It was not until 1848 that the relationship between the pancreas and blood glucose levels was revisited.
One of the pioneers was the physiologist Claude Bernard (1813-1878). While operating on the gastrointestinal tract of dogs, he tried to ligate the pancreatic ducts, which eventually led to the destruction of the pancreas.
Another interesting observation was made in 1870 by a French physician, Apollinaire Bouchardat. He noticed that malnourished patients during the siege of Paris in the Franco-Prussian War of 1870-1871 miraculously began to feel better (because their glucose levels plummeted).
The discovery of insulin
The careful study of the pancreas was the work of Joseph von Mering and Oskar Minkowski. After the complete removal of the pancreas of an experimental dog (it is a pity that the name of this character was not preserved in history), the dog developed diabetes: glycosuria (the presence of glucose in the urine) combined with polyuria, marked hunger, weight loss, and asthenia were noted. When they transplanted a small remaining piece of pancreas with a vascular pedicle subcutaneously in the area of the anterior abdominal wall, the diabetes stopped developing. This fact finally confirmed that the pancreas produces "something" necessary for the regulation of carbohydrate metabolism.
French researcher Edouard Laguesse localized the source of the secretion in 1893. He noticed small clusters of cells in the pancreas that played an important role in the digestive process. These clusters were named "islets of Langerhans" in honor of their discoverer, Paul Langerhans. In 1869, Paul Langerhans first described these clusters of cells as distinct from the underlying pancreatic tissue.
A little later (and almost simultaneously), Jean de Meyer, a Belgian scientist, and Edward Albert Sharpey-Schafer, an English scientist, noticed that the islets of Langerhans release a secret — a hormone called insulin (from the Latin insula, "island"), which promotes the accumulation of glycogen in the liver.
With the study of the role of the pancreas came the idea of modeling similar organic processes. Georg Ludwig Zülzer isolated an extract from the pancreas of rabbits, dogs and calves, which he called “Acomatol.” This extract was given to several diabetics, one of whom was in a coma. Surprisingly, the patient even woke up, but then he was overcome by side effects — fever, weakness, allergies.
More important were the experiments conducted by the Romanian scientist Nicolae Paulescu (1869–1931) on a diabetic dog. The four-legged patient was injected with serum from the pancreas of another dog. This serum was called "pancreine" by Paulescu. The dog got better, but Paulescu (due to laziness or poor time management) did not publish his results in time, so the Nobel Prize went to other scientists.
In 1921–1922, a group of Toronto scientists — professors Sir Frederick Banting and John J.R. Macleod, chemist James Collip, and graduate student Charles H. Best — succeeded not only in synthesizing the hormone insulin, but also in demonstrating its effects. At first, they acted like Paulescu, suggesting that the lack of the hormone be compensated for by consuming pancreas or an extract isolated from it. However, this had no effect because insulin is destroyed before it even enters the body. An article by Moses Barron led to new experiments, in which it was noted that the islets of Langerhans were not destroyed when the pancreatic ducts were ligated (this was also noticed by Leonid Sobolev [1876–1919] in Russia). Later it turned out that it was possible to obtain pancreatic extract even faster and easier by using underdeveloped bovine fetuses, in which the gland was already functioning, but not yet producing external secretory cells. In this case, bandaging anything was not necessary.
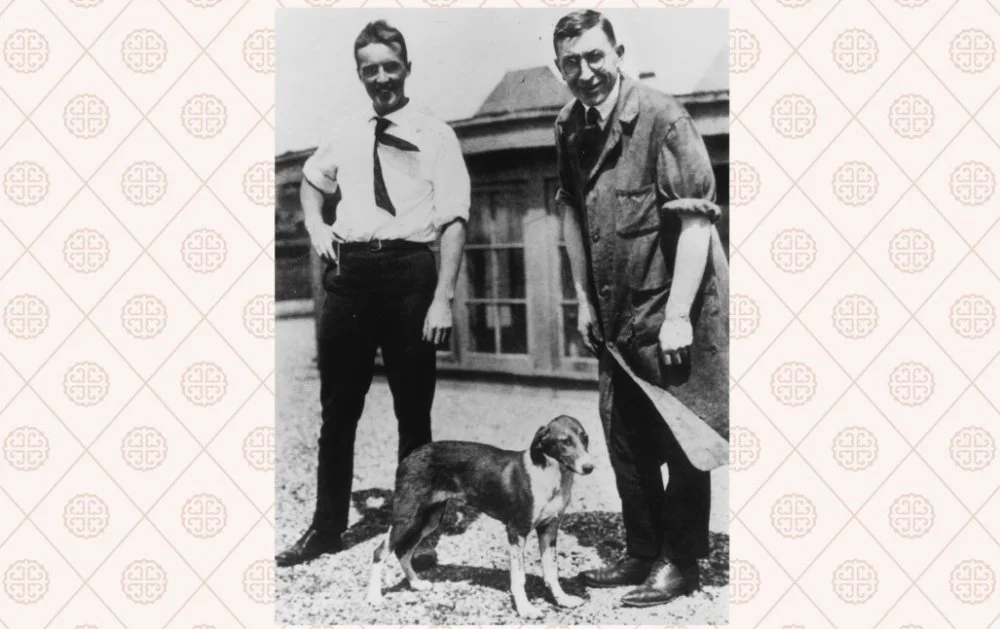
Charles Best and Frederick Banting with a diabetic dog / Photo by Hulton Archive/Getty Images
The dog trials were successful, and scientists began testing on humans. In early January 1922, doctors at a Toronto hospital injected pancreatic extract into a 14-year-old boy with severe diabetes, Leonard Thompson. The injection produced only a slight reduction in blood sugar and glucosuria levels, without affecting the clinical picture, and caused the formation of a sterile abscess, i.e. suppurative inflammation. The treatment was stopped immediately. Then James Collip joined the experiment and suggested improving the extract by making it more concentrated. Leonard received another injection, this time an improved one. The results were immediate: blood sugar levels dropped to normal and the ketonuria (characterized by weakness and excessive urination) disappeared. Leonard Thompson lived on insulin for another thirteen years and died on April 20, 1935, at the age of 27, from bronchopneumonia and other complications of diabetes.

Leonard Thompson. The first patient to receive an insulin injection / insulin.library.utoronto.ca
Bunting and Macleod won the Nobel Prize in Physiology or Medicine in 1923. Best was not on the list. Frederick Bunting (whose birthday, November 14, is recognized worldwide as World Diabetes Day) was furious and even threatened to refuse the award, but was persuaded not to. He gave half of the money he received to Charles Best and publicly acknowledged his contribution to the discovery of insulin. It was Charles who did all the "physical work" — operating on animals, administering injections, etc. Macleod, for his part, acknowledged that Collip had done no less for the success of the experiment, so he gave him part of his fee. Thus, none of the actors involved in the creation of insulin were financially deprived.
Wanting to make life easier for as many diabetics as possible, the scientists sold the patent for their invention to the University of Toronto for the symbolic sum of one dollar. However, insulin was too expensive to produce and distribute, so the university soon sold the patent to pharmaceutical companies.
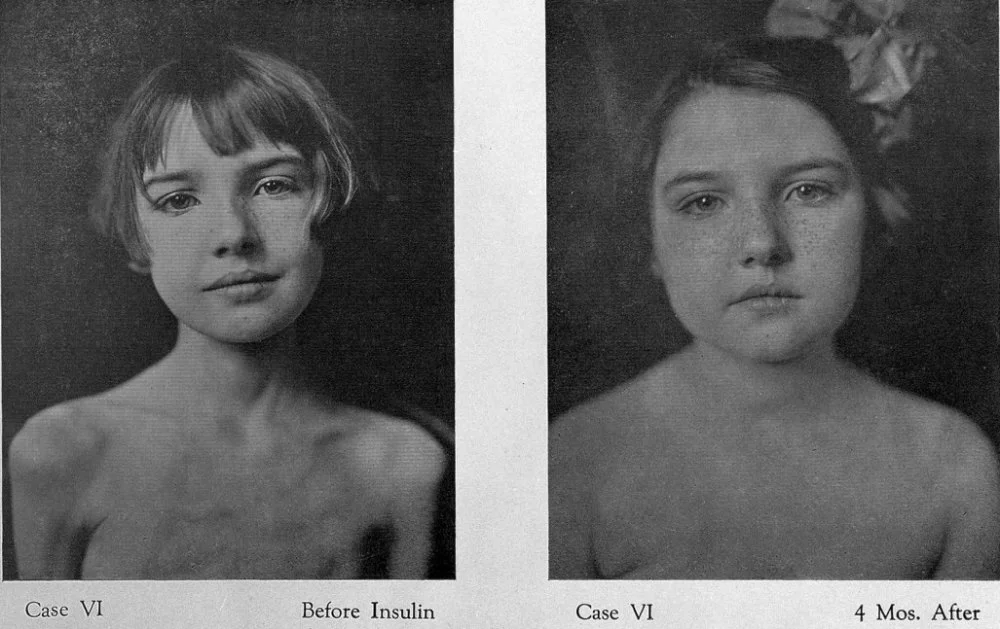
Diabetic girl before and after insulin injection / Welcome Collection
Two major manufacturers emerged, Lilly in the United States and Novo in Denmark. In 1946, Novo employee Hans Christian Hagedorn discovered NPH (Neutral Protamine Hagedorn) insulin, which prolonged the action of the drug and allowed diabetics to take fewer injections. This invention, however, could not meet the rapidly growing demand for insulin. It became expensive and time-consuming to purify pig pancreas extract. Ways had to be found to synthesize the drug in vitro.
Frederick Sanger's discovery of the amino acid sequence of human insulin in 1951, for which he received the Nobel Prize in 1958, was a breakthrough. This method is often referred to as genetically engineered insulin, indicating how it is produced.
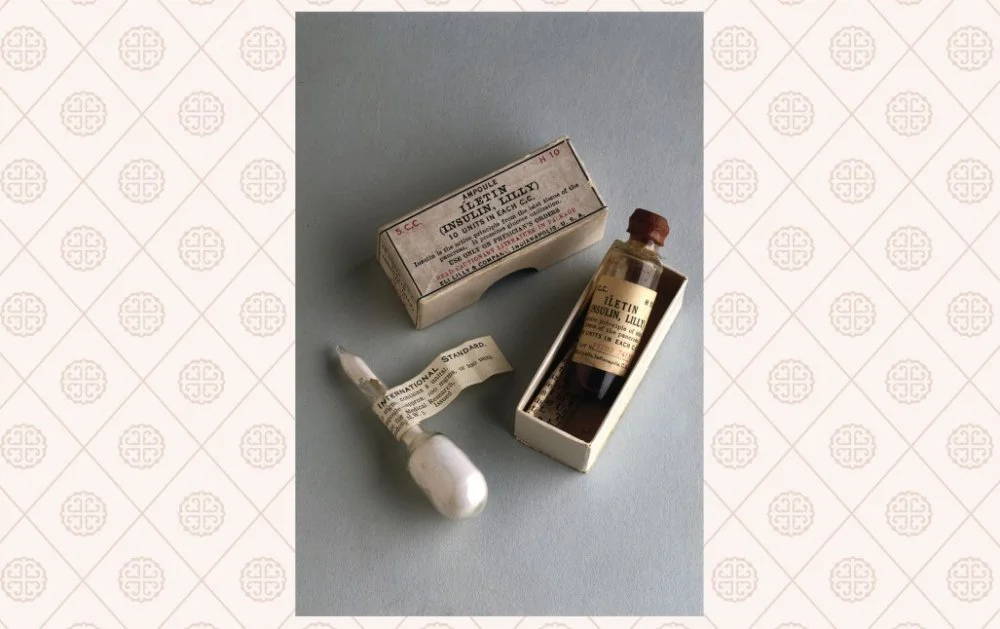
An insulin ampoule in 1923 / Photo by SSPL/Getty Images
Then came recombinant insulin. It is produced by strains of yeast and E. coli in a special nutrient medium. In this case, the amount of the substance obtained is so high that it makes it possible to completely abandon the use of products derived from animal organs.
By the 1980s, insulin had become ubiquitous in the treatment of diabetes; insulin pumps, syringes, and pens began to appear.
Today, there is even talk of eliminating injections and switching to pills. In 2019, in the United States there was information that Semaglutide (Ozempik) in tablets was approved. In 2022, scientists from Nizhny Novgorod, Russia, also patented insulin tablets. This is convenient, because it saves a person from the need to constantly carry syringes and solutions for injections.
References
1. Maggie B. Covington, MD. Traditional Chinese Medicine in the Treatment of Diabetes // Diabetes Spectr. No. 14 (3), 2001, pp. 154–159.
2. Gemmill CL. The Greek concept of diabetes // Bulletin New York Academy Med., No. 48 (8), 1972, pp. 1033-1036.
3. Герасименко О.А. Оскар Минковский — открытие, изменившее мир. // Сахарный диабет. № 11 (4), 2008, с. 102-103.
4. Karamanou M, Protogerou A, Tsoucalas G, Androutsos G, Poulakou-Rebelakou E. Milestones in the history of diabetes mellitus: The main contributors. // World Journal of Diabetes, No. 10:7(1), 2016, pp. 1-7.
5. Poretsky L. Principles of Diabetes Mellitus. Springer: New York, 2010.

