Miscellaneous
Curious facts about beauty, culture and worldview of people
Special projects

RUBIES, SAPPHIRES, AND OTHER CARBUNCLES
Gems and People: A Dramatic Story of Love and Misunderstanding
~ 12 min read

THE GREAT NEEDLEWORK RACE
The History of Olympic Fashion
~ 11 min read

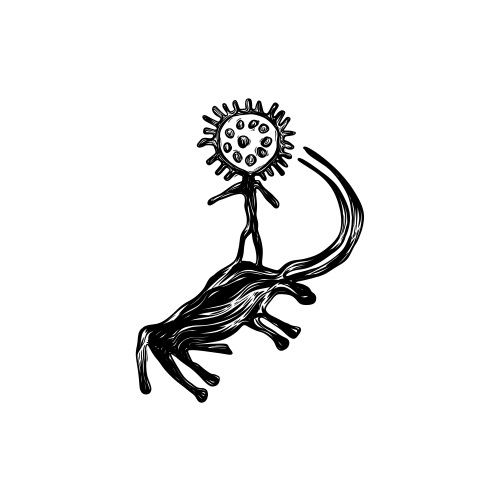
ABYLKHAN KASTEEV’S NAÏVE SOCIAL REALISM
Between the beauty of life and the power of ideology
~ 11 min read